The QIDP
A blog by and for QIDP's, QDDPs', Case Managers and all those who have been a QMRP at one time or another.
Tuesday, September 20, 2022
H.R. 8863 "Words Matter Act"
Most people working in the field of Intellectual Disabilities left the words "Mental Retardation" in the dust a long time ago. Even before Rosa's Law A Short Look at Rosa’s Law and What it Changes many people had dropped the terminology from daily use. Those deciding not to use the outdated and misued terms, started using terms such as "People with disabiliites" or "Disabled individuals" or one of the best, just "People." Now, over ten years since President Obama signed Rosa's Law, "Mental Retardation" is still being used in U.S. Code and by many in public. It's not unsual to find a physician or psychologist still clinging to the diagnosis of "Mental Retardation." It's not really any one person or groups fault, the words "Mental Retardation" have been in use since the 1960s and have been a cornerstone of diagnosis since that time.
Rosa's Law came into being not because "Mental Retardation" was a bad term, but because it was a misued term. The words was often modified and used in slang and for crulty. People would say things like "You're so 'retardaded" or "You're a retard" and many other variations. Ironically, it was the same misues of medical terminaology that caused "Mental Retardation" to be implemented in the 1960s. Prior to that period of time, dianogisis for people with Intellectual Disabilities was based on words like "Idiot," "Moron," and "Imbecile." If you're like me, you likely cringed when you read those words, but before the 1960s, they were in common use and very accepted by society and the medical field. Unfortunately, those words were also in common misuse.
Perhaps the best thing to say about H.R. 8863 "Words Matter Act" is "it's about time." Rosa's Law has been in place for over ten years. Most of us in the field have moved to the use of "Intellectual Disabilities" or "Developmental Disabilites" for our reports, terminology, and everyday use. It's time for the government to catch up with the rest of us.
Much like the 1960s and 2013, I suspect that in the future "Intellectual Disabilites" will be misued. I do not think this is the last time society will have to address the misuse of a medical diagnosis for slang and name-calling. It seems like society has to address this issue about every fifty years. While I will not likey be around to see the next transition for the diagnosiis, it would be nice to hope for a time when laws do not have to be implemented to address the slang and misuse of a diagnosistc word for a disability which affects so many beautiful and outstanding people.
Tuesday, January 25, 2022
COVID and The Future
Let's face it, COVID is here to stay. Regardless of the removal of masks mandates, the return to routine life, and even the fight to keep public schools open, COVID is still touching people's lives around the nation. Some have mild cases of a COVID, while others face life-threatening mutations and the potential of life on a vent. A person may have a mild case of COVID with no symptoms, and six months later, that same person may end up in a hospital. There is simply no way to tell at this point how COVID may affect you.
We are still in the reporting stage for COVID and the Infection Control stage in Texas. An ICF facing a COVID outbreak - defined as one resident or one staff having a COVID positive test result - must call the reporting hotline. Once the facility calls the reporting hotline, they are told to email the report to the state through the reporting system. The steps for reporting and results of that report have been explained in several provider letters, but a brief review is:
1. Call to report - get told the email to send the report to Austin.
2. Report to the email address providing the needed information such as vendor number, etc.
3. Continue infection control procedures and follow your facility plan.
4. Within 5 days, send in the investigation report.
5. Usually, within 24 hours, expect an on-site visit from HHSC to review your Infection Control procedures.
Because COVID is constantly changing and mutating, the above procedures in Texas are not likely to go away anytime soon. Therefore, self-Reporting, Infection Control, and entry screening will be the norm for some time to come.
As a facility, there are several things you can do to help minimize a COVID outbreak. First, all facilities should consider the following:
1. Is the infection control procedures up-to-date and effective?
2. Are we continuing to screen visitors, staff, and others entering the home - and documenting it?
3. Are we watching for signs of COVID?
4. Have residents been vaccinated, and have they received a booster?
5. Has the benefits of vaccination been explained to staff and offered?
6. Is the facility prepared for an outbreak - for example, is a plan is in place?
If we continue to focus on Infection Control, training, and we are prepared to act when a test is positive, we can get through this crisis. The road ahead will be long and hard, but with proper preparations and planning, there will eventually be a time when we see COVID level off and perhaps even become a rarity instead of the norm.
Thursday, January 21, 2021
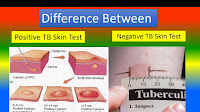
COVID Vaccine Might Cause Positive TB Test
As we move quickly through the new vaccine and await the results of vaccinations, more issues are being found. One concern is the COVID vaccine could trigger a positive TB test result. As of this writing, I have been advised that at least one facility administered the vaccine and, within a few days, completed their annual TB skin test only to have almost everyone test positive.
A quick search on the Internet revealed that the CDC is aware of the issue. There are already several articles addressing the problem as well (example: Article).
A nurse for the facility where the TB test was completed and showed positive after the vaccine recommends updating the TB test first. Most facilities such as ICF programs obtain an annual TB test. If your facility is scheduling a COVID Vaccine, it might be advisable to update all TB tests for the year first. To get specific recommendations or instructions, discuss this with the facility nurse or medical advisor.
Sunday, January 3, 2021
Vaccine Information for ICF/IID Providers
Although the state and CMS have not issued any formal guidelines for administering the vaccine to people living in ICF programs - i.e. what consents you may need - there is a "Best Practice" model you may want to consider.
For programs I work directly with, we are taking this approach in Texas. First, we obtained the side effects. This can be found on the FDA website as a "Fact Sheet" midway down the page (FDA Website). I took the following actions:
1. Obtained the Fact sheet
2. Developed a consent for the vaccine
3. Attached fact sheet and consent form:
a. Guardian review and signature
b. SDM review and signature
c. IDTeam review and signature
d. or Individual review and signature if competent
4. Consent was then reviewed by the IDTeam
5. Consent, IDTeam review then reviewed by the Specially Constituted Committee or Human Rights Committee.
While I may be going overboard, I feel like it is better to cover it so there are no questions.
You will need to keep in mind that the vaccine comes in two doses. According to current sources, the vaccine does not end the need for social distancing, mask, and other precautions. The state has also not issued any information (Texas) as to when or if mask and precautions can be stopped after the administration of the full vaccine.
Information on Vaccine:
FDA website with vaccine information
Friday, December 4, 2020
COVID Helpline for People with Intellectual Disabilities and Caregivers
Just before Thanksgiving, The Arc of California and the Stony Brook University School of Social Welfare launched a helpline for people with Intellectual Disabilities and caregivers. The helpline may be utilized by families, caregivers, support teams, and individuals as needed.
The helpline was developed to provide support to those suffering during the COVID-19 Pandemic. The helpline is available 24 hours a day for support, counseling, and help as needed to anyone. Support, guidance, and referrals will be made as needed.
Known as "Project Connect," the service is open to anyone needing assistance or simply wishing to talk. The number is 888-847-3209.
In addition to Project Connect, many individual states have already set up assistance helplines, webpages, and information. A simple Internet search will reveal many and can be targeted to your specific state or region.
The United States International Council on Disabilities also provides an extensive list of resources at this address: United States International Council on Disabilities.
Saturday, September 19, 2020
COVID-19 Isolation Impact on People with Intellectual Disabilities
People with Intellectual Disabilities have been isolated for hundreds of years, and COVID-19 has just set that isolation factor back by fifty years. Anyone looking at the history of the ICF/IID programs - Intermediate Care Facilities for Individuals with Intellectual Disabilities will realize that COVID-19 has pushed back our timetables to at least the mid-1960s.
In the United States, during the 1950s through the mid-late 1970s, isolation of people with Intellectual Disabilities (ID), at that time called "Mental Retardation," was the standard practice. If someone had a diagnosis of ID, he or she was routinely referred to a large institution. Often, referral to a large institution meant separation from family, the public, public schools, and even public places such as physician offices, churches, and clinics. In fact, that isolation even extended beyond death in some cases with isolated morgues and graveyards located on institutional campuses. A person with ID could go his or her entire life without ever having contact with anyone outside of staff and peers in their home setting.
The exposure of Willowbrook literally shocked the world and especially the United States. In the 1960s, Civil Rights movements had focused on equality for all people. This equality meant equal assess to public accommodations such as physicians, hospitals, schools, and other public places. While the implementation of the Civil Rights was still in process and can be argued to still be on-going even today, it was apparent from the Willowbrook state facility in New York that people with ID had been overlooked. Out of this oversight came dozens of federal programs, including the ICF program, designed to get people with an ID diagnosis out of institutions and into community access.
Since the 1970s through the 1980s, 1990s, 2000s, states across the nation have worked to meet people's rights and access with ID. Things like grocery shopping, church attendance, access to public schools, college, and public facilities and services such as physicians, libraries, and parks have worked to accommodate people with ID. Inclusion became the keyword. IDTeams (Interdisciplinary Teams) worked to find ways to secure community inclusion. The work completed during this time set new standards, broke down barriers, and opened doors. Suddenly people with ID were no longer being separated, segregated, or ignored. Suddenly, people with ID graduated from local high schools, participated as board members, lived in communities, attended church, visited with their doctors at the doctor's office, and even set up final preparations and were buried with other non-disabled people in local graveyards. In a few decades, separation and seclusion were replaced with community inclusion and participation in life.
In March of this year, the unthinkable happened. A pandemic of COVID-19 spread rapidly across the United States and devastated the community's inclusion progress. Most states almost immediately "Locked Down" long-term care facilities. These emergency precautions instantly affected the ICF. Suddenly there were no church services, schools were closed, shopping was not allowed, and even something as simple as a trip to McDonald's was limited to a drive-thru.
In Texas, ICF programs were required to have staff wearing PPE. The people with ID, living in their own homes, were and still are, required to wear face coverings when out of their rooms. No visitors were allowed. No unnecessary trips or medical follow-ups were permitted. The state quickly enforced new Infection Control procedures, isolation procedures, and quarantine procedures.
The effects had the outcome that anyone would and should expect. After decades of having their rights, freedoms, and community inclusion ignored then finally given by the government, the government came in and removed those rights, freedoms, and community inclusions. In a simple fact, the government took away the one thing that so many people with ID cherished. Was it right? Was it wrong? Who knows the answer as history will have to judge our generation for what was done in the name of protecting people. The fact is, the government did not take away those rights, freedoms, and inclusions lightly, and it was done with the best of intentions to protect people with ID. Only now, ICF programs are just starting to have the opportunity to "Open Up" again with specific plans in place.
While it may have been the right thing to do and it may very well have been needed, the fact remains the people with ID have had the hardest time dealing with this crisis. Some have been happy and understood the need for restrictions. Others have cried and literally screamed because they miss family, friends, church, outings. The staff and those working in the field continue daily to talk, counsel and reassure that this restrictive atmosphere will not last forever. Regardless of the facts surrounding COVID-19 and the restrictions that had to be placed, the bottom line remains that we have set people living in ICF programs back by fifty years or so in their collective timeline. Their battle for rights, freedoms, and community inclusion is perhaps fresher than any other population living in the United States. Maybe it's the fact that the rights, freedoms, and inclusion they gained so recently were impacted so soon needs to be remembered the next time anyone considers restricting them and how those restrictions are implemented.
Tuesday, August 25, 2020
Monday, August 3, 2020
Testing Numbers in Texas May Be Off - Here's Why...
The realizations of the potential for double counts came during a conversation between county health officials and the administrator for the facility. The administrator was asking questions in regard to PPE and other issues related to staff when the county official expressed appreciation for the list received. Surprised, the administrator said, "I am working on the list now. I have not sent it in yet." The county official then pulled the list for the facility and found that the lab had reported the test results and completed the county forms. With a large number of facilities reporting, it is possible that without this type of conversation, the county could have counted the facility residents twice.
If we are looking at drastic numbers in nursing facilities, we need to be aware that the lab and the facility both reporting can double the numbers on record. The average ICF is six beds in Texas so this could increase a count up to twelve if everyone in the home was infected. This may not sound like a great number, but if we consider a little over 800 ICFs in Texas, then those numbers become scary. If all 800 (rounded) ICF programs were six beds and all had COVID-19, the numbers should be at 4,800 cases - again assuming everyone in each six-bed facility had COVID-19. Now, if the county is getting numbers from the facility and the lab, those numbers double. Instead of 4,800 on the books, you would have 9,600 positive cases of COVID-19.
It is doubtful that you can coordinate with your lab and keep them from reporting. Most facilities, when speaking with the county officials, should discuss the possibilities that the lab and the facility may both be putting out the same numbers. If you make your county coordinator aware of the problem, it may help ensure the number count is more accurate.
Wednesday, July 15, 2020
Happy Developmental Disabilities Professional Day
 |
| Logo for Developmental Disabilities Professionals Day |
The day is more than just a "QIDP" day though. This day is meant to recognize all professionals in the field. We are talking about the psychologist, psychiatrist, nurses, directors, case managers, social workers, service coordinators, surveyors, and so many more. There are titles from QDDP to QIDP to Medicaid Worker to Service workers all given to people working with people. The impact these professionals make is extraordinary.
Let's face it, we each have responsibilities. Often the direct care staff implements the plans written by the professionals. It may be a behavior plan to help improve social skills, or it could be a medication plan to maintain health and well being, or any other dozens of plans. These plans come from professionals. Though planning, observations, input from individuals, family, friends, and others, the Developmental Disabilities Professional from the Medical Doctor to the Case Manager develop plans with profound impacts on the lives of people. The responsibility is great. A medical procedure or medication today could extend a person's life for years. A plan today to teach someone how to hold a job, move into the community, and even manage money could one day made the difference between dependence and independence.
Developmental Disability Professionals put in long hours and years of work. They often give up family time, stop eating at restaurants, leave a movie, ballgame, or concert early all because the call comes to rise to a professional level, and serve. Sadly, some of those professionals will never see the impact their work has accomplished. Through changing jobs, moving people, changing programs, and simply years, what is taught or worked toward today, may not be realized until long after the professional has left the scene.
Maybe you will never know the change you have affected, or maybe you will. Maybe one day after your time here is finished, you will arrive in the next world. You may be greeted by a long line of people you do not recognize, but yet something is familiar about them. They will no longer have developmental disabilities. They will no longer be confined to wheelchairs, braces, or other supports. They will no longer have a diagnosis, a condition, or a problem of some other kind. Maybe you will meet these people in that next life, and they will tell you the stories of how your work changed their lives in this world. These will be the people free of disabilities because God will have finished the work you started here. You are important and there can be no higher calling than to serve people.
Wednesday, July 8, 2020
Behind the Scenes at Texas HHSC Surrogate Program
Over the years, the staff has come and gone in the Austin office for the Surrogate Program. The program is currently overseen by two individuals. Dennis Tomlinson and Marti Granger receive the request for Surrogate service from the entire state of Texas.
Dennis and Marti are responsible for the implementation of the program, according to Texas law. This means they must gather the initial information, which includes paperwork like Certifications of Need, Data forms, notification forms, etc. In addition to a list of standard forms from Texas, the two must also gather information about specific procedures or medications. The information needed can include medical histories, family histories, social and psychological histories, nursing notes, psychiatric notes, or dental and medical notes. It ultimately depends on what procedure or request is being made to the program as to what documentation will be required.
The program currently only addresses needs in an ICF/IID setting. The areas covered are major medical treatment, major dental treatment, administration of psychoactive medications, and the use of highly restrictive behavior procedures. Also, the program may include the release of records to assist in obtaining consent and decisions the IDT indicates may pose a risk to individual protection and rights.
Outside of Dennis and Marti, the program depends entirely on a network of volunteers. Volunteers attend a training - usually with Dennis or Marti - and learn the limitations under the law, the rules, and how to conduct hearings for a person from an ICF/IID program.
Perhaps the most crucial aspect of the entire program is the gathering and reviewing of the information for each person served. Dennis and Marti must ensure that all information possible is gathered, reviewed, compiled, and distributed for a hearing. The information, should it ever be needed, must show that the program administrators gathered all possible answers, avenues, and potential outcomes for the volunteer to use in making a decision. The process and responsibility fall entirely to Marti and Dennis in the background.
Often providers and volunteers alike forget there is a considerable amount of work that goes on before a hearing. Some hearings can last forty-five minutes or an hour or so, but the work that has gone into the preparation sometimes takes weeks and months to come together. In the diligence required to ensure all aspects of a case are presented for review, Dennis and Marti have the sole responsibility. It should be remembered that the work they do impacts the ability to make informed decisions for people. In the area of making informed decisions, there can be no higher calling that requires so much care as ensuring the people we serve have a fair and knowledgeable hearing. In the shadows of each hearing held, two people can be seen. From time-to-time, those two people deserve a spotlight, and a thank you for the service they provide to the people living in ICF/IID programs.
Wednesday, May 27, 2020
Stimulus May Arrive as a Debit Card
The card instructions state "Shop anywhere Visa Debit Cards are accepted..." and "Get cash back at the register with PIN..." Anyone with the card can access it. These cards are pre-loaded with $1200 or $2400 depending on the individual's status. The cards were sent with no previous notice and appear to be arriving for people on Social Security and other benefits at this time, however, it is unclear to the general public at this time exactly who will receive the cards.
Initially, we were told that those living in nursing facilities or receiving SSI would receive a paper check or direct deposit depending on what information the IRS has regarding the person. The paper check, as indicated before, saw some facilities having the residents sign them over. This signing over of the checks is still being investigated in some areas. A debit card brings an entirely new aspect and list of concerns to the table for ICF providers and others. Some of the concerns that must be considered:
1. Accountability - who will account for the card, the spending on the card, and records for the card? How will the facility prove a resident used the money and someone else did not?
2. Lost cards - as we all know our residents in an ICF are here for care and assistance. They are sometimes forgetful, and sometimes they misplace items. The facility needs a plan to ensure no debit cards are lost - once lost anyone with the card can use it and it is very possible the IRS will not replace it.
3. Moving the money - the money on these cards can be used or moved into an account. Moving into a trust fund would likely be the best bet; however, it has to be clearly documented where the money came from and that it was stimulus money. This will help avoid the $2000 limit on accounts and allow this to not account as assets. Keep in mind though, there is no clear direction from the IRS, CMS, or most states yet regarding what documentation may or may not be required to maintain the money as stimulus funds moved from debit cards. There will need to be a way to ensure it does not appear simply as cash on hand during an audit or a Medicaid review - hopefully, more guidance in this area will be forthcoming.
4. Theft - Unfortunately the fact is sometimes we hire people willing to steal from our residents. It's sad but true. Much like accountability above, there needs to be a system in place to ensure the card does not benefit staff or anyone else other than the resident receiving it.
Each facility administration needs to be on the lookout for these cards in the mail. I would suggest that if one is received, the manager, staff, or person receiving it at the home should notify the administration immediately. An IDTeam meeting for ICF homes will likely need to be held and the above four areas addressed by the team with the resident to ensure we protect funding for the people we serve.
Tuesday, May 19, 2020
Stimulus and Medicaid Limits
Friday, April 24, 2020
CDC Rolls Out Mask and Screening Requirements for COVID-19
Many providers in Texas received emails this afternoon indicating the new requirements were in place. Here is a brief summary:
1. ICF staff must wear a mask while on duty in the facility. Failure in Texas according to HHSC to comply will result in deficient practice as an Infection Control deficiency.
2. ICFs must screen all visitors and staff for signs of COVID-19. This screening must include surveyors, consultants, staff, owners, family, or anyone entering the facility.
3. Failure to screen, according to CMS, will result in an Immediate Jeopardy (IJ) deficient practice deficiency.
ICF/IID programs should take away several things from these notifications and assume potential visits are pending. With the new requirements, a facility that has been visited in the past may be visited again very soon. The facility should immediately ensure masks are available and being used by all staff. Screening must be done for potential COVID-19 issues. The final thing to take away from this is the seriousness that HHSC and CMS have placed on the issue. For the state to indicate that failure to screen will mean an immediate IJ, shows just how serious of a threat we are facing. One program manager reminded facilities that over 9,000 long term care residents have died due to COVID-19.
Thursday, April 9, 2020
Infection Control Survey Visits in Texas
First, let's look at the basic facts- The ICF/IID program was not around during the last major Pandemic of this proportion - 1918-1920. In fact, many of the agencies we have today providing regulations and oversight were not around during the Spanish Flu of 1918-1920, and indeed, we have no staff with experience from that Pandemic. So it must be kept in mind that providers, state and private, HHSC, and CMS is really treading into new territory. With any move into new territory, there is always a learning period. There is also a lot of "helpful" opinions floating around. There are naturally people on all sides of the ICF/IID world with strong feelings as to how this Pandemic should be monitored, handled, and what specific responses are needed. Because there are so many different views, we are going to see things happen that we agree with and some that we do not agree with happening on all levels. Let's face it, some providers have no idea what they are doing right now, and some oversight would likely be helpful. Some providers have extensive systems in place that includes temperature checks, no visitors, and even questionnaires before staff can enter the home. Other homes are depending on staff to be open and say, "Hey, I'm sick," and that's all they are doing. Needless to say, as with all disasters, we are all learning. The bottom line, there are people on all levels with no real experience or knowledge, so we have to learn as we go.
The second thing we must keep in mind is that CMS is directing HHSC to do these survey visits. In almost all visits I have heard about or reviewed, the surveyors have been professional, apologetic, and fast in their tours. Just to be truthful, they do not want to be in the home just as the home providers do not want them there. Nobody wants to be potentially exposed to this virus. Some surveyors are even apologizing to the homes and saying they understand and wish they did not have to come out right now. But, we have to keep in mind that standards - federal and state as well as the new E tags for just such disasters - are in place as a minimal procedure to keep the people we serve safe. We also have to keep in mind that all facilities make mistakes - if they did not, then we would see deficiency-free regular surveys yearly! But, because we all make mistakes, surveyors need to come into the homes and monitor, point out the errors according to regulations, and allow us time to put corrective measures in place. That is precisely what is happening now- surveyors are coming out to review and ensure that we - the providers- are doing everything possible to safeguard the people we serve. Let's face it, sometimes things are overlooked, forgotten, and sadly by some providers simply ignored. That is the primary reason we need an outside set of eyes to come in and review, point out those concerns, and when necessary, write deficient practice so we can correct and improve our services. This period is no different - it's all about ensuring the safety and well-being of the people we serve in the ICF programs. For that alone, we should accept the fact that surveyors need to touch base with us and view the plans right now.
So far, typical Infection Control Surveys have been reported to focus on Infection Control policies of the home, supplies in the house, PPE in the home, procedures, and training with staff on handwashing, visitor procedures, and community access policies or procedures during this time. They have also questioned staff ratio plans, how the facility will handle a potential staff having COVID-19, and if the facility is following reporting requirements. Surveyors are asking how the facility is handling informing the people served about the Pandemic - i.e., why are you not going to the workshop, why are you not all going to Walmart, why can you not have visitors right now, etc.?
It can undoubtedly be frustrating for a facility that has taken safeguards and steps to ensure the protection of the people served to have a surveyor walk up to the door. The general feeling that seems to be shared is, "We have limited visitors and outings and have no outside contact, and here comes a surveyor with a potential to spread this virus from home-to-home in the front door!" It's a valid concern, but unfortunately, it is a need. Just as we have to depend on staff to come and go from the facility, administration, nurses, QIDPs, etc., we also have to expect that surveyors will need to check on our status. It is not an intent to spread COVID-19, and there is no conspiracy going on to undermine procedures put in place. All surveyors so far seem to be following whatever access procedures the home has in place - which may include temperature checks, questions about travel, and even some are requesting the surveyor wear a mask. So, the facility needs to view the surveyor as just another "essential" staff person entering the home just as we would all the other people needed to keep the house functional. We must always remember, the safety and well-being of the people we serve in these homes must be the priority, and I personally think that is precisely the priority of CMS and HHSC with these Infection Control Surveys.
Wednesday, March 11, 2020
Staff and The "Did I do that?" Syndrome
In the 1980s, there was a Friday night comedy where one of the main characters was always making huge, although unharmful, mistakes that made the other cast members look bad. Whenever that character would be confronted by his fellow cast members, usually with something like, "Steve" drawn out with the sound of frustration, Steve would respond, "Did I do that?" His voice was squeaky, annoying, and the audience almost always looked for it in each episode. The remark, "Did I do that," was funny. It became a household saying for a lot of kids when they got in trouble. Sometimes, it seems that our staff in the ICF should be responding in the same voice, "Did I do that" when they do things less than expected. The supervisors are usually left shaking their heads and wondering what staff was thinking when they acted. You can hear the rise of the voice, "Did I do that," as all concerned end up amazed.
Unfortunately, the "Did I do that" moments almost always occur during the annual survey. The administration team receives the deficient practice list with words like, "DCS A took client 1 to the living room to clean his face," or "DCS B left the bathroom door open while assisting client 3." Whatever the case may be, the supervisors have usually found themselves asking, "Why did you do that?" The end result is a POC, monitoring, training, and staff being instructed to "never do that again."
The fact remains though that many of the staff working are good...indeed many of them are great. So, why do they make these mistakes that result in deficient practice, and the "Did I do that" syndrome? There are actually several potential reasons:
1. Staff was never trained on how a procedure needs to be done to be compliant with standards.
2. Nobody monitored staff regularly to ensure issues or concerns were addressed.
3. It may have been some time since the last training and staff may have forgotten.
4. Someone else said, "This is how we do it," even though how they showed "it" was wrong.
5. Staff may just not care.
If you read the above potential reasons, you will find a common factor in all of them. No Supervision intervention is seen. An old saying that a friend of mine used a lot is "People do what you inspect, not what you expect," and she is right.
1. If the staff is never trained, whose fault is that? Supervisors.
2. If nobody monitors the staff and offers correction, whose fault is that? Supervisors.
3. If there are considerable gaps in training dates, whose fault is that? Supervisors.
4. If another staff showed the new staff the wrong way, whose fault is that? Supervisors.
5. Finally, if the staff does not care and they are working, whose fault is that? Supervisors.
As you can see, unless your supervisor is involved with staff, when that staff takes a person served to the living room to brush his teeth, or wash his face, right in front of the state surveyor, then that supervisor has no place to complain to anyone. The fact is, the supervisor failed in some way.
Do you want to cut down on the "Did I do that" moments? If you do, then get your supervisors involved. Have them train, monitor, and train again regularly. If they do this, your issues in this area will drop, or you will find out quickly that you have a staff that simply may not care. If you have the staff that does not care, then maybe its time for that staff to find another area for work.
Saturday, May 4, 2019
When Do You Have Too Many Assessments?
If you have ever gone through a survey or an investigation with a state agency, then you know there is a chance the person conducting the survey will ask for assessments. Most of the time the request will be for a specific assessment. The surveyor may want to see an assessment by the nurse, the physician, or even something by the direct care staff if the investigation involves a specific area in the facility. For example, the person served may have been playing basketball outside, the ball rolled out into the street, and the person ran after the ball and got hit by a motorcycle. We'll assume the person is okay, just a little banged up. What assessments will the surveyor ask for during the investigation? They will likely ask for the nurse assessment and the physician's assessment for sure. You'll answer questions like, "Has this person ever done this before?" "What safety precautions are you taking to ensure it does not happen to him again?" and "How are you going to make sure it doesn't happen to anyone else?" Finally, the surveyor will look at you and ask that additional, and sometimes surprising question, "Do you have a community access assessment or an assessment like it for street or traffic safety?" This is where some providers have the "Deer in the headlight" look. They go through their policy book, nope there's no assessment like that there. They then talk to the QIDP - "So, do we have community access or traffic safety assessment?" The QIDP gives that funny look - kinda like the Deer look - and says, "No, we've never needed one."
So, you return to the surveyor and tell them you do not have an assessment like that. Why do we not have that assessment? Well, the standards did not list it - or at least did not explicitly say, "Community Access" or "Traffic Saftey," but the facility obviously needed one. The next thing you know you have a new assessment and everyone in the facility is being assessed on his or her "Traffic Safety."
If you go through the above type situation enough times, you're going to have a ton of assessments. You're going to have safety assessments, cooking, cleaning, traffic, swimming, shopping, crowd response, etc. You may find one day that you have an entire book of nothing except assessments. Naturally, some of the assessments will be required, but some of them will be situationally and placed only to ensure a problem from the past does not occur again.
So, if we circle back to our original question, "When do you have too many assessments" the answer really and truly is, never. There is likely a reason for each assessment you have, and there will be a reason for each one you add in the future. The truth of the answer is you must look at each individual person you serve in the ICF not only as an individual but on an individual basis.
Your IDTeam has a lot of authority in this area. The answer is to, no pun intended, assess the need for any assessments not required annually. For example, let's go back to the community access assessment. You have a person you serve who is in a wheelchair, can not move it himself, and never wants to go anywhere. Does that person need a community access assessment? Well, maybe he needs one initially, but after that, if there are no changes, perhaps he does not need one annually. On the opposite side, let's say the person walks daily to the store but has stepped in front of cars or crossed against the traffic before in the past - he may need an annual assessment and goals to address the issue.
The driving factor here is that you do not have to use all the assessments your organization may have. You can take each person as an individual and decide what assessments need to be done annually - provided they are not required annually by standards - and move forward. You only have too many assessments when the IDTeam decides one is not needed for someone.
Tuesday, November 27, 2018
Texas ICF Consents
There are roughly 700-800 ICF/IID programs in Texas and all have a need for consents to meet the federal and state standards. Sometimes the two, federal and state, can appear to be at odds with one another, but regardless of your view on that issue Texas has a specific avenue to obtain consent for just about any issue. In the ICF, you need consent to spend money on a t-shirt up to consent for psychotropic medications. I work with facilities that have upward of five different types of consents depending on the person's ability (client).
There is an easy way to decide what type of consent is needed in Texas. You have only a handful of avenues as described below:
- Guardian - no matter what age the guardian gives the approval for just about everything including psychotropic medications.
- Surrogate Decision Maker - an involved family member can give consent for just about everything except psychotropic medications and certain medical procedures - but very limited in that area.
- Person - the person (client) can give consent if the IDTeam has assessed them to have the ability to give informed consent.
- IDTeam - when a person can not give consent, the IDTeam can give consent for things like spending, and daily needs, but can not for medical issues, psychotropic medications or highly restrictive procedures (usually restrictive behavior plans, etc.)
- Supportive Decision Maker - not really making a decision, but providing the information to the person (client), giving him or her options and then providing the person's answer back to the IDTeam - this helps when a person needs support to make decisions.
- Surrogate Decision Making Committee - a group of volunteers through the state makes decisions on anything not reserved for the Surrogate Decision Maker, or the IDTeam - can make decisions on psychotropic medications, medical procedures, and restrictive procedures.
Friday, July 27, 2018
Make a Difference Again
Many years ago I watched a Star Trek movie that featured both the famous Captain Kirk and Captain Picard. During one scene in the movie, Kirk asked Picard, "Are you close to retirement?" in which Picard answered, "I hope not." Then Kirk asked, "Are they going to promote you?" and Picard answered, "Not that I'm aware of." At that point, Kirk said, "Don't. Don't let them retire you, don't let them promote you because as long as you sit in that chair, you can make a difference." The movie goes on to eventually have Picard challenge Kirk to "Make a difference again," and so goes the movie, but the point was that as Captain of the ship, Picard did not have to do everything, but he had to "Coordinate" and oversee the "Services" of the entire ship. Those decisions, his knowledge, and his commitment to his crew can be akin to the knowledge and commitment a QIDP has to have to the clients...the people, that he or she serves. It doesn't matter whether you are a QIDP for one year, ten years or twenty years, the fact is as Kirk said, "...as long as you sit in that chair, you can make a difference."
It's been a while since I posted an article here. I would like to think its because I've been "Making a difference," or more importantly Changing Lives. Perhaps the more narrow view to take would be to promote the question, "Am I changing a life?" If the answer is "yes," then I'm doing not only my job, but I'm making a difference. If on the other hand, the answer is "No." Then it's time to take the same challenge that Picard issued to Kirk..."Make a difference again".
Remember, as long as you sit in that chair, you're the QIDP and you can make a difference...you can change lives for the better. It takes work, it takes dedication, it takes knowledge, but the reward is a life changed for the better and not much can beat that.
Tuesday, September 19, 2017
The Importance of Life Safety Code Surveys for ICF/IID Programs
Monday, August 7, 2017
Intellectual Disabilities and Openings in the ICF/IID Programs in Texas
Intellectual Disabilities and Openings in the ICF/IID Programs in Texas